Non-motor symptoms are those that are not related to movement. They range from physical effects like trouble swallowing or pain to mental and emotional impacts such as depression, apathy and anxiety.
Symptoms can happen at any time and can even start before a PD diagnosis is made. Often they can be managed with the same anti-Parkinson drugs that improve movement symptoms.
Cognitive Impairment and Psychiatric Symptoms
While the four cardinal motor symptoms of PD (bradykinesia, rigidity, postural instability and tremor) get most of the attention, it is important to recognize that the disease also affects the mind, senses, sleep and mental health. In some cases, these non-motor symptoms appear years or decades ahead of the development of PD’s movement-related symptoms.
These non-motor symptoms include a loss of the sense of smell (olfactory dysfunction or hyposmia), constipation and gastrointestinal problems, urinary incontinence, depression or anxiety, drooling, cramped or small handwriting and trouble thinking and concentrating. These symptoms are often the first noticeable signs of PD and may even serve as an early warning sign.
These symptoms are common and can significantly reduce quality of life in PwP. Many are treatable and can be managed using lifestyle changes, medications and complementary therapies. Embracing wellness strategies, getting good sleep and practicing stress management are all helpful to minimize the impact of these symptoms on mood.
Autonomic Dysfunction
Autonomic dysfunction is a common non-motor symptom in PD and can severely compromise quality of life. Symptoms include problems with heart rate, gastrointestinal and urinary symptoms and sweating.
The latest Movement Disorder Society clinical diagnostic criteria for PD retain bradykinesia and rest tremor as the core motor features but emphasise that non-motor symptoms are also common and can significantly worsen the quality of a person’s life. This reflects new insights and understanding about the nature of PD, and its progression, and emphasises the need for better management of these symptoms.
Symptoms of dysautonomia include a variety of conditions including orthostatic hypotension, abdominal pain, irritable bowel syndrome, constipation, sweating abnormalities and vasovagal syncope (the involuntary fainting caused by the response to stress). They can be triggered or worsened by many medications used for PD such as anticholinergic drugs, dopamine agonists and tricyclic antidepressants. They can also be exacerbated by underlying conditions such as diabetes and some chronic illnesses like Ehlers-Danlos syndrome.
Sleep Disturbances
Fatigue is one of the most common non-motor symptoms of Parkinson’s disease. It can make it hard to fall asleep at night and causes a lack of energy throughout the day. It may also be aggravated by medication side effects or other factors, such as stress or depression.
Sleep problems may include trouble falling asleep, frequent waking during the night, and a general feeling of not getting a good rest. They can be exacerbated by other PD symptoms such as pain, tremors, and drooling.
Some people with PD develop restless leg syndrome (RLS). RLS is an uncomfortable feeling in the legs that is relieved only by movement. People with PD can also have nocturnal hallucinations, which may include disturbing images or sounds. Others experience REM sleep behavior disorder, which causes them to act out their dreams in their sleep. This can include violent actions and vivid dreams, which can be alarming to family members.
Fatigue and Energy Conservation
Fatigue is a common symptom of PD, and it can have a significant impact on quality of life. It can be defined as a pervasive sense of tiredness that is not relieved by rest or sleep and interferes with mental or physical activities. It can also be associated with depression and anxiety (Upneja et al, 2021).
Fatigue often develops later in the course of PD and is more common in those taking dopamine agonist medications, particularly ropinirole/Mirapex and pramipexole/Requip. It has been shown that fatigue is related to changes in basal ganglia dopamine function and changes in brain connectivity, suggesting it may be a compensatory strategy for basal ganglia dysfunction.
To help reduce fatigue, plan daily tasks to match your energy levels and limit the number of activities you attempt in one day. Incorporate a regular exercise program to improve fatigue and keep muscles well-conditioned.
Pain Management
While scientists work on new treatments, doctors can help manage your Parkinson’s non-motor symptoms today. They can advise you on when to seek care for problems like trouble swallowing (dysphagia), incontinence and fatigue.
A doctor may use a variety of therapies to help manage PD non-motor symptoms, including biofeedback, in which you place painless sensors on your body to learn how to control bodily functions, such as heart rate. In addition, some patients benefit from cognitive-behavioral therapy, which teaches you to change how you think and act.
There’s increasing evidence that PD non-motor symptoms can be early warning signs of the disease and that they can start years before motor symptoms appear. In fact, the first signs of PD often involve non-motor symptoms, such as resting tremors and cogwheel rigidity. Seek treatment for these signs as soon as possible. You’ll need to take your medications on a regular schedule to be most effective.
Sensory Symptoms
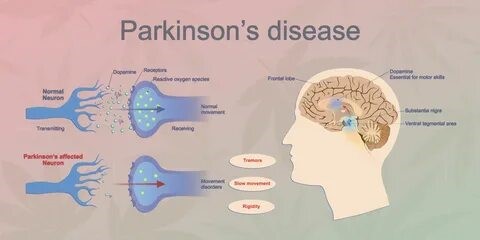
A lack of dopamine affects how your brain sends activation signals to your muscles and also fine-tunes movements. This is why PD causes movement symptoms like tremors and stiffness.
In addition to motor changes, PD can cause sensory problems. A loss of smell (hyposmia) and a reduction in the sense of touch are common. Other sensory changes include a loss of balance, double vision and a dry mouth.
There are many tests to diagnose PD, but experts know less about non-motor symptoms of the disease. One test involves a spinal tap, in which a healthcare provider inserts a needle into your spine to collect cerebrospinal fluid for testing. This will look for misfolded alpha-synuclein proteins that can increase your risk of PD. The other test includes collecting a sample of your skin, including nerve cells that are near the surface. This is called a skin biopsy.


